This post is for informational purposes only and should not be used in place of the advice of a medical professional.
As we age, our bodies undergo various changes, some of which can lead to unexpected health concerns. One such issue commonly faced by older adults is leg swelling, also known as edema. This condition can range from being a mild inconvenience to a serious health problem, depending on the underlying causes.
Understanding the key factors behind leg swelling in the elderly is crucial for effective management and prevention. In this blog post, we will explore the primary causes of leg swelling in seniors, providing you with valuable insights to help you recognize, address, and potentially prevent this common issue.
Key Takeaways:
- Leg swelling in elderly people can result from various causes, including chronic venous insufficiency and heart conditions.
- Lifestyle changes, such as using compression stockings and regular exercise, can help manage symptoms.
- Consulting a healthcare provider is essential for diagnosing the underlying cause and determining the appropriate treatment plan.
Leg swelling is a common issue among elderly individuals and can be caused by various factors. Chronic venous insufficiency is one of the most common causes, where blood doesn’t flow properly through the leg veins, leading to fluid buildup. Other possible causes include heart conditions like congestive heart failure, which can cause fluid retention and swelling in the lower extremities, as well as kidney problems and liver disease. Swelling of the legs can also be a symptom of deep vein thrombosis, a serious condition where blood clots form in the deep veins of the legs.
In older adults, lifestyle changes and management strategies can help reduce symptoms. This includes using compression stockings to improve blood flow and reduce swelling. Regular exercise and reducing salt intake can also help manage fluid retention. Seeking medical advice from your healthcare provider is crucial to determine the underlying cause and receive the appropriate treatment plan. Managing chronic swelling effectively can improve your quality of life and reduce the risk of further health problems.
Understanding Leg Swelling

Leg swelling, or edema, often occurs due to fluid buildup in the lower legs and can indicate various underlying health conditions. This can involve the blood vessels, veins, and lymphatic system.
Definition and Overview of Edema
Edema refers to the swelling that happens when excess fluid gets trapped in your body’s tissues, especially the lower extremities. Peripheral edema is the medical term for swelling of the legs, ankles, and feet.
A common cause of leg edema in older adults is chronic venous insufficiency. Varicose veins and prolonged periods of standing or sitting can also lead to swelling. Chronic health conditions like congestive heart failure, kidney disease, and liver disease might contribute to fluid retention. Edema symptoms often include leg swelling, aching, difficulty walking, and pitting (a condition where pressing the swollen area leaves a dent).
Anatomy of Leg Swelling
In the legs, blood vessels and the lymphatic system are crucial in managing fluid balance. When blood vessels and capillaries are damaged or weakened, they can leak fluid into surrounding tissues, leading to leg swelling.
The lymphatic system helps drain fluid that leaks out of blood vessels. Problems with the lymph nodes or lymphatic vessels can cause fluid buildup and swelling, known as lymphoedema. Conditions like deep vein thrombosis can block blood flow, causing swollen legs.
Compression stockings and lifestyle changes like increasing physical activity and reducing salt intake can help manage symptoms. Medical conditions like heart disease, kidney problems, and high blood pressure may require specific treatments under a healthcare provider’s guidance. Compression therapy and water pills (diuretics) might also be part of the treatment plan for reducing swelling in the lower limbs.
For any sudden or severe leg swelling, especially if accompanied by chest pain or shortness of breath, seek immediate medical attention.
Common Causes of Leg Swelling in the Elderly
Leg swelling in elderly individuals can result from various health conditions. This can include cardiovascular issues, kidney or liver problems, and inflammatory responses due to infections.
Cardiovascular Issues
Chronic Venous Insufficiency is a common reason for leg swelling in the elderly. The veins in your legs have trouble sending blood back to your heart, causing fluid buildup, especially in the lower legs and ankles. This can lead to varicose veins and chronic swelling over time.
Congestive heart failure occurs when your heart doesn’t pump blood effectively, leading to excess fluid in your legs. High blood pressure can also stress the heart, worsening symptoms. Pulmonary embolism, a blood clot in the lungs, may cause sudden, severe leg edema and requires immediate medical attention.
Kidney and Liver Concerns
Kidney disease and chronic kidney disease disrupt your body’s ability to regulate fluid, causing fluid retention in the lower extremities. When your kidney functions poorly, it fails to remove extra fluid, leading to swelling. Nephrotic syndrome, a kidney disorder, can increase this swelling.
Liver disease, such as cirrhosis of the liver, hampers blood flow through the liver, leading to fluid buildup and edema in the legs and abdomen. Lower albumin levels from liver disease can also contribute to fluid retention and swelling.
Kidney failure requires careful monitoring. If you have signs like chest pain or shortness of breath along with leg swelling, seek medical advice. Blood tests can help diagnose kidney problems, guiding your treatment plan.
Inflammation and Infections
Peripheral edema often results from inflammation in the tissues of your legs. Infections, such as cellulitis and fungal infections, can cause the affected area to swell. Redness and pain often accompany this swelling.
In addition, conditions like deep vein thrombosis, where a blood clot forms in the deep veins of the legs, can lead to significant swelling and pain. Lymphatic system problems can cause lymph nodes to swell, contributing to fluid buildup and chronic swelling in the legs, making it hard to walk.
Epsom salts, compression stockings, and regular exercise can help manage inflammation. Staying active prevents poor circulation and helps to reduce the symptoms of edema. Consulting your healthcare provider is important to address the underlying cause and prevent further damage.
Lifestyle Factors and Diet
Certain lifestyle choices and dietary habits can significantly impact the occurrence and severity of leg swelling, particularly among older adults. By paying attention to nutrition and maintaining physical activity, you can manage and even reduce symptoms of edema.
Effect of Nutrition on Edema
Eating a diet high in salt can lead to fluid retention, worsening leg swelling. Reducing salt intake is crucial to manage leg edema. Processed and salty foods contribute to excess fluid in your body.
Foods rich in sodium can cause your lower legs to swell more due to increased blood volume. Focus on a balanced diet with plenty of fruits and vegetables.
Hydration is also essential. Drink enough water to help keep your lymphatic system working efficiently. This prevents fluid buildup in your legs. Avoid excessive consumption of alcohol and caffeine as they can dehydrate and affect blood flow.
Maintaining a proper diet aids in reducing high blood pressure, another contributing factor to leg edema and other health issues like congestive heart failure and kidney problems.
Weight and Physical Activity
Maintaining a healthy weight is critical. Being overweight and obesity can put extra pressure on your lower limbs, making it harder for blood vessels to circulate blood efficiently. This can exacerbate leg swelling and cause varicose veins.
Regular exercise, such as walking or ankle pumps, can improve blood circulation in your legs. It helps prevent fluid from pooling in your lower extremities. Physical activity promotes overall health and can relieve symptoms of poor circulation.
For those who have difficulty walking, low-impact activities and specific exercises can still be beneficial. Spend less time sitting or standing in one position. Compression socks or stockings are another effective tool. They help reduce swelling and improve blood flow in the lower legs. Consult your healthcare provider to develop a suitable treatment plan.
Specific Conditions Leading to Edema
Various health conditions can lead to leg swelling, particularly among elderly individuals. Notable causes include issues related to pregnancy, disorders of the venous and lymphatic systems, and certain medications or substances.
Pregnancy-Related Swelling
Pregnancy often leads to swelling in the lower legs due to fluid retention and hormonal changes. Pregnant women might notice ankle swelling and discomfort, particularly in the later stages of pregnancy.
The extra fluid and blood needed to support the growing fetus can cause a buildup of fluid in the lower extremities. This is more pronounced after long periods of standing or sitting. Compression stockings can help reduce symptoms, as can elevating the legs. However, sudden and severe swelling could indicate a more serious condition, like preeclampsia, and should be evaluated by a healthcare provider immediately.
Venous and Lymphatic System Disorders
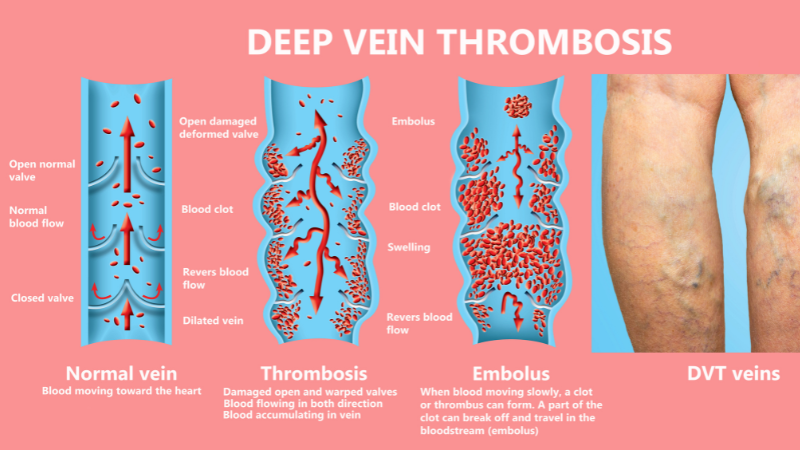
Disorders in the venous and lymphatic systems contribute significantly to leg edema in older adults. Chronic venous insufficiency (CVI) is a common cause. Here, blood struggles to return to the heart due to weakened or damaged valves in the leg veins, leading to fluid buildup that results in swelling.
Other conditions, such as deep vein thrombosis (DVT), where a blood clot forms in a deeper vein, typically in the lower leg, can obstruct blood flow and cause significant swelling. Untreated DVT can lead to serious complications, including pulmonary embolism.
Lymphedema, caused by damage to or removal of lymph nodes, inhibits proper drainage of lymphatic fluid. This leads to swelling in the affected area, often the legs. Treatment options include compression therapy, exercises to encourage fluid movement, and in some cases, surgical intervention.
Medications and Substances
Several medications can lead to edema as a side effect. Nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, calcium channel blockers, and some antidepressants are among the medications that can cause fluid retention.
Diuretics, or water pills, sometimes prescribed to reduce swelling, may also lead to complications if overused. The improper balance of fluids and electrolytes can worsen swelling or create additional health issues.
Patients on medications such as those for high blood pressure or heart disease should monitor for leg swelling and consult with their healthcare provider to adjust their treatment plan if necessary. In some cases, lifestyle changes, like lowering salt intake and regular exercise, can mitigate the side effects.
Diagnosis and Evaluation

To identify the cause of leg swelling in elderly individuals, healthcare providers conduct thorough assessments, including physical examinations and specific tests to detect underlying conditions.
Clinical Assessment
A physical examination is crucial to assess leg swelling. Your healthcare provider will evaluate both lower limbs for signs of redness, warmth, and differences in size between the legs. They will also check for varicose veins and other visible abnormalities.
Checking for symptoms of a blood clot, like deep vein thrombosis, is essential. If you report chest pain or shortness of breath, immediate medical attention is needed to rule out serious conditions like pulmonary embolism. Swelling in the ankle area, combined with heart issues, may indicate congestive heart failure, requiring a detailed cardiovascular examination.
Your doctor might ask about your medical history, looking for conditions such as liver disease, kidney problems, or high blood pressure, all common in older adults. Lifestyle factors, such as long periods of inactivity or poor nutrition, might also be discussed to understand the cause of the leg swelling.
Testing for Underlying Conditions
Various diagnostic tests help in identifying the root cause of leg swelling. Blood tests can be used to check for kidney function, liver disease, or other underlying health problems. These tests provide essential insights into your overall health.
Imaging tests, like an ultrasound or Doppler study of your leg veins, help visualize blood flow and detect any blockages or chronic venous insufficiency. In cases of suspected heart failure, a chest X-ray may be ordered to evaluate heart size and possible fluid buildup in the lungs.
Lymphatic system evaluation can reveal issues related to fluid retention and peripheral edema. If your healthcare provider suspects more severe conditions like nephrotic syndrome or cirrhosis of the liver, more advanced tests may be required for a precise diagnosis.
Treatment often depends on the specific diagnosis. For example, compression stockings or water pills might be recommended to reduce excess fluid. Identifying the underlying cause is key to developing an effective treatment plan.
Management and Treatment Strategies

Managing and treating leg swelling in elderly individuals involves lifestyle modifications, medications, medical procedures, and supportive therapies. These strategies address both the symptoms and underlying causes, such as chronic venous insufficiency, congestive heart failure, and kidney problems.
Lifestyle Modifications
Simple changes can significantly reduce leg swelling among older adults. Dietary adjustments are crucial; reducing salt intake can decrease fluid retention and lower blood pressure. Maintaining a balanced diet rich in fruits, vegetables, and lean protein supports overall health and reduces inflammation.
Regular exercise like walking and ankle pumps enhances blood circulation, preventing fluid buildup in the legs. Elevating the lower limbs above heart level for short periods throughout the day can help decrease excess fluid and reduce ankle swelling.
Using compression stockings or compression socks can also be effective. They support leg veins and improve blood flow, helping to manage symptoms of edema.
Always consult a healthcare provider before starting any new exercise or dietary changes to ensure they are safe and suitable for your health conditions.
Pharmacological Interventions
Medications play a pivotal role in treating leg edema. Diuretics, or water pills like furosemide (Lasix), help remove excess fluid from the body, reducing swelling. These are commonly prescribed for conditions like chronic kidney disease, congestive heart failure, and cirrhosis of the liver.
For those with high blood pressure, calcium channel blockers might be necessary. These medications prevent fluid buildup and potential complications like pulmonary edema. It’s essential to follow the prescribed treatment plan and regularly consult your doctor to adjust medications as needed.
In some cases, underlying health problems such as deep vein thrombosis or infections may require specific treatments like antibiotics or anticoagulants. Regular blood tests and physical examinations can monitor the effectiveness of these medications and manage any side effects.
Surgical and Medical Procedures
In severe cases, surgical and medical procedures might be required. Surgical treatment for varicose veins, such as laser therapy, can improve blood flow and reduce chronic swelling. For those experiencing severe complications from conditions like kidney failure or liver disease, more invasive procedures like catheterization or dialysis may be necessary.
Early intervention in serious conditions like a pulmonary embolism is crucial. Immediate medical attention, often involving chest x-rays and other diagnostic tests, can prevent further damage to the body and manage symptoms of edema effectively. Healthcare providers might also consider procedures to remove lymph nodes or repair damaged blood vessels if they significantly impact lower leg circulation.
Supportive Therapies
Supportive therapies can complement other treatment options to reduce swelling and discomfort. Applying compression therapy with compression socks or stockings helps manage edema by improving circulation and reducing fluid buildup in the affected area.
Physical therapy is also beneficial, especially for elderly individuals with mobility issues or difficulty walking. A physical therapist can design a program that includes gentle exercises to strengthen muscles and improve leg circulation.
Additional home remedies like soaking feet in Epsom salts can provide temporary relief for swollen lower extremities. Ensuring good skin care can prevent complications like fungal infections or further damage from prolonged swelling. Staying hydrated, but monitoring the amount of water intake, is also essential in managing symptoms effectively.
Consult your healthcare provider to tailor these supportive therapies to your specific needs, ensuring they align with your treatment plan for optimal results.
Prevention and Long-Term Care
Preventing leg swelling in the elderly involves managing underlying health conditions and regular monitoring. Long-term care focuses on both reducing excess fluid and maintaining blood flow in the lower legs.
Monitoring and Ongoing Management
Regular monitoring of leg swelling can help you catch issues early. Keep track of the affected area and skin conditions. Watch for symptoms of a blood clot, such as sudden swelling or chest pain.
It’s essential to manage chronic health issues. Regularly check your blood pressure and control your salt intake. Wear compression stockings to improve blood flow in the veins. Elevate your legs to decrease fluid retention in the lower limbs.
Use diuretics or water pills as directed by your healthcare provider. These help reduce fluid buildup caused by conditions like congestive heart failure or chronic kidney disease. Keep an eye on side effects and consult your provider about any new symptoms.
Education and Research Advancements
Stay informed about the latest developments in the field of leg edema. Research shows that chronic venous insufficiency and varicose veins are common causes of leg edema in elderly adults. Exercise your calf muscles to support blood circulation and strengthen the veins in your lower extremities.
Publications from the Mayo Clinic and similar institutions provide helpful information on managing these conditions. Engage in regular physical activity and maintain a healthy lifestyle to support long-term vascular health.
Educational material from healthcare providers can offer tips on recognizing warning signs. Knowledge about deep vein thrombosis and other serious conditions is crucial.
Research advancements continue to improve treatment options, from better compression therapy techniques to new medications. Stay in touch with your healthcare team for updates.
Conclusion
Leg swelling in the elderly can result from a variety of causes, ranging from benign lifestyle factors to more serious medical conditions. By identifying and understanding these key factors, you can take proactive steps to manage and mitigate the effects of edema.
Regular check-ups, maintaining a healthy lifestyle, and promptly addressing any health concerns with your healthcare provider can significantly reduce the risk of leg swelling and improve overall well-being. Remember, staying informed and vigilant is essential to ensuring the health and comfort of yourself or your loved ones as you navigate the aging process.